Reposted from The Verge
Sept 11, 2020
By Nicole Wetsman
At the Eddie Warrior Correctional Center in Oklahoma, over 90 percent of inmates have tested positive for COVID-19. Nearly every facility in the Oklahoma prison system has been touched by the virus, says Nicole McAfee, director of policy and advocacy at the ACLU of Oklahoma. She assumes that they still haven’t seen the worst of it — and to make matters even more complicated, flu season is about to start.
The flu regularly spreads through prisons and jails in the US for some of the same reasons that COVID-19 does. The facilities pack vulnerable people in close quarters, with limited access to soap or other ways to protect themselves against an infectious disease. Handling a single outbreak is already a struggle in these places, which often don’t do enough to protect the health of the people living in them. Now, they may have to handle two.
“The idea of trying to mitigate and treat against potential simultaneous flu spread and COVID-19 spread seems relatively terrifying,” McAfee says.
VACCINATION ACCESS
One of the best ways to manage the flu is through the flu shot, which helps prevent people from getting sick and can make the illness less severe in people who do catch it. Public health experts are pushing everyone to get flu shots this year because lower levels of flu will leave the health care system with more resources to manage COVID-19. In some prisons and jails, though, getting a flu shot can be difficult.
“There’s absolutely no consistency across the board,” says Lauren Brinkley-Rubinstein, an assistant professor of social medicine at The University of North Carolina at Chapel Hill studying health and incarceration.
The Federal Bureau of Prisons recommends that all staff and inmates be offered a flu shot and that priority should go to older inmates or inmates who have chronic health conditions. But those guidelines don’t mean most inmates in the US get flu shots; outbreaks regularly happen in prisons where most inmates aren’t vaccinated. In 2011 in Maine, two prisons that vaccinated fewer than 10 percent of inmates had outbreaks. In 2018, a woman died of the flu in an Oregon prison that only gave flu shots to 18 percent of inmates.
Access to a flu shot is even more unlikely in jails because people usually only stay in them for a few days. The short length of stay makes offering a shot more challenging, Brinkley-Rubinstein says. “But I also think that is not good enough justification, especially in the context of COVID-19, where we’ve seen these major outbreaks in jail settings,” she says.
People tend to cycle in and out of jails, so offering them a flu shot helps protect both the jail population and the wider community, says Tyler Winkelman, a health policy researcher at the Hennepin Healthcare Research Institute in Minnesota. “There will be many people who would benefit from the influenza vaccine who go to a jail, and they should have the ability to get a flu shot when they’re there,” he says.
Winkelman also works as a physician at the Hennepin County jail. Anyone brought into that jail is offered a flu shot during intake, he says. “We’ve already started offering it,” he says. “We have multiple opportunities for people to be asked about it if they decline it during intake.”
The health clinic at the Hennepin County jail is unique, though: it functions more as a community clinic that happens to be at a jail. It allows physicians to use resources available anywhere in the health system, which is not the case in most jails. “I would guess that many jails will have challenges in being able to offer people influenza vaccines,” Winkelman says.
FIGHTING TWO OUTBREAKS
If flu outbreaks do happen in prisons and jails already facing cases of COVID-19, the challenges those facilities are already facing could be compounded. In Oklahoma, the resources in many jails and prisons are already stretched thin fighting the coronavirus, says McAfee. She’s been hearing rumors that staff, especially medical staff, are leaving Oklahoma prisons because the work conditions are dangerous or because they’re getting sick themselves. “I just wonder, then, how people are going to get the care they need,” McAfee says.
A lack of medical staff would make it especially hard for jails and prisons to sort people with COVID-19 from people with the flu in order to give them the right treatments. The symptoms can be similar. “Symptom screening, especially during flu season, is not going to cut it,” Brinkley-Rubinstein says.
The best way to differentiate between the two diseases is by testing, Winkelman says. But access to testing resources for COVID-19 varies widely from jail to jail and from prison to prison. “There are some jails that are equipped to do this well, and others that really just don’t have the resources to test everyone who should be tested,” he says.
Some of the procedures put in place to prevent the spread of COVID-19 in jails and prisons could, theoretically, help stave off major influenza outbreaks. But those policies have, in many places, been unsuccessful. COVID-19 still caused devastating outbreaks in dozens of facilities around the country. Over 100,000 people who are incarcerated have tested positive for the virus.
The widespread COVID-19 outbreaks pose another problem. After watching those outbreaks unfold for months, inmates may be reluctant to cooperate with health staff, which could complicate flu mitigation efforts. Men in California’s San Quentin State Prison told The Verge that they don’t trust prison officials, who they think let the coronavirus in intentionally. They may also not report symptoms or agree to testing if saying that you’re sick means moving to an isolation area, Brinkley-Rubinstein says. “You might be put into a quarantine setting that sure looks a lot like solitary confinement,” she says. Since the start of the COVID-19 pandemic, the use of solitary confinement in US prisons has gone up 500 percent, according to research by the nonprofit group Solitary Watch.
The overlap of COVID-19 and flu is a threat to prisons and jails for many of the same reasons it’s a threat in the wider community: any other respiratory disease drags desperately needed resources away from the pandemic. It’d add more illnesses to an already struggling system.
On top of that, prisons are filled with people who are more likely to have underlying health issues than people in the general population. Those people are vulnerable to COVID-19 and are also more at risk of a severe case of the flu. “Folks who are incarcerated are generally at higher risk of worse outcomes,” Winkelman says.
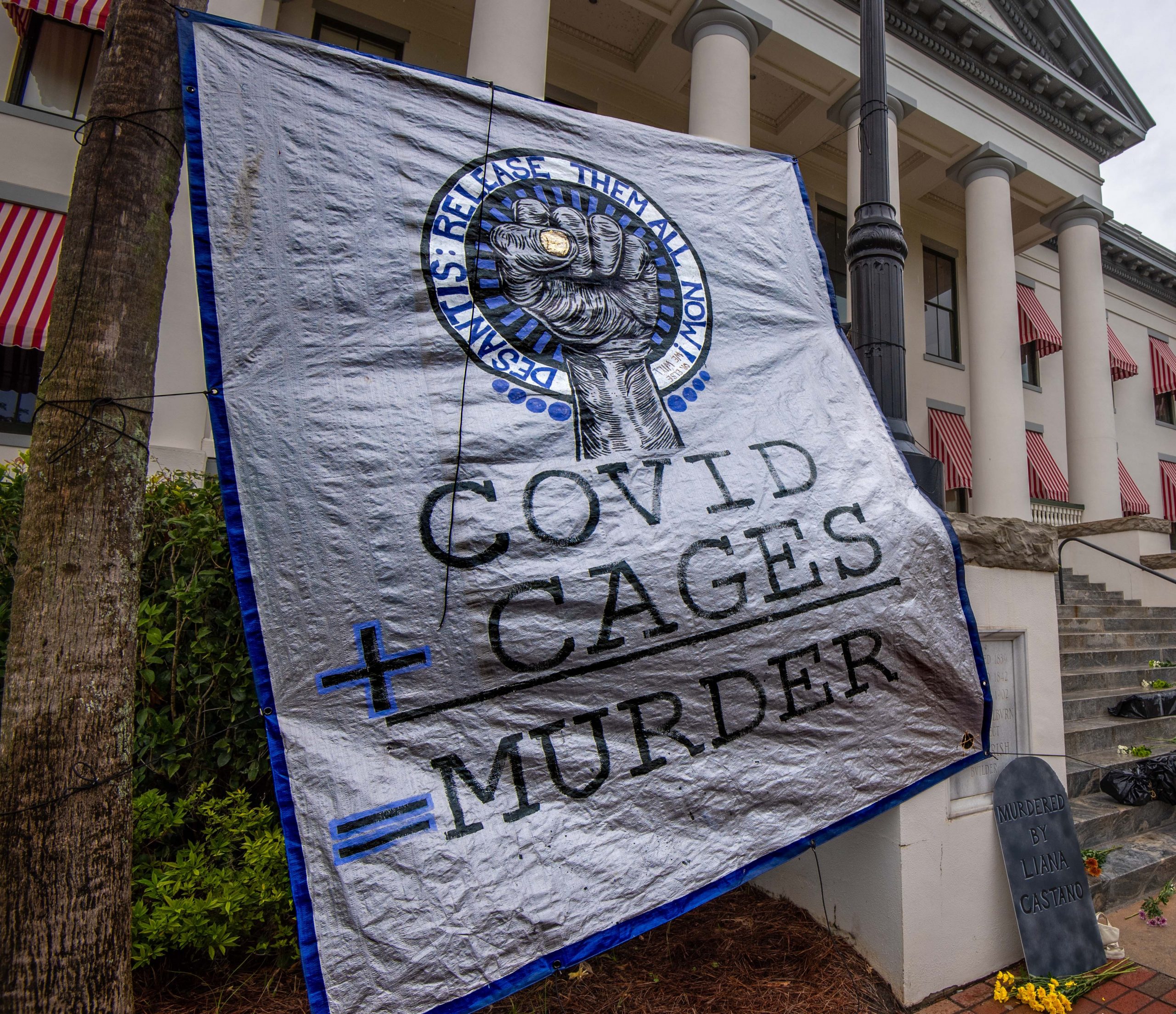
The best way to protect people in prisons and jails from the dual threat is to release them from the facilities, Brinkley-Rubinstein says. Public health experts have recommended prisons and jails reduce their populations since the start of the pandemic. Some facilities made slight reductions early on, though they weren’t sufficient to stop COVID-19 from spreading in many cases. Now, months into the pandemic, some facilities are starting to steadily repopulate back to the levels they had in March, she says.
In order to have the safest-possible flu season during an active pandemic, it’s important to think of prisons and jails as a part of the community — not separate from it, Winkelman says. Efforts to reduce flu in prisons and jails matter for the health of the general population, and vice versa. “It’s all part of our overall ability to test and treat people during the influenza season,” he says.